Work Package 4: Intervention Development
The vision for WP4 is to develop and feasibility test a new set of interventions based on a participatory system dynamics approach (PSDA) to prevent diabetes in selected high-risk target groups defined in WP2. This approach was chosen over the highly protocolised and expert based approaches applied to diabetes prevention so far with disappointing long-term impact. The interventions will be developed in co-creation with citizens, families, local organisations, councils and health care providers to achieve sustainable diabetes prevention. Implementation will be across selected regions, municipalities and local communities in Denmark, Greenland and the Faroe Islands in order to create local and sustainable solutions to prevent type 2 diabetes.
The PSDA process combines current evidence on prevention and health promotion, best practice and local insights to achieve new knowledge and create feasible and sustainable solutions/interventions for a complex health challenge such as diabetes prevention(1,2). This approach implies that a variety of engagement and solutions may occur at both the interpersonal and organisational levels. Hence, addressing health in a systems approach, rather than at an individual level only, is novel in the sense that it acknowledges that changes in one aspect of the system can have ripple effects throughout the entire system(3,4). We hypothesise that developing co-created intervention(s) inspired by psychosocial theories such as motivation, health literacy, social support and social networks and based in the local community setting/family setting, will result in sustainable improvements in behaviour (diet, physical activity, sleep) and wellbeing and thereby prevent development of diabetes in people at high risk (WP2).
Several researchers at SDCA, SDCC and SDCS have substantial experience with PSDA in different settings and target groups in Denmark. Employees from all participating SDCs will receive training in how to apply PSDA to solve complex health challenges regarding diabetes prevention. The target group for the training is regional consultants and employees from the selected local communities (e.g. local communities in a municipality) taking part in the development phase.
PSDA process components
Stage 1: Preparation phase
Review of existing evidence and practice regarding diabetes prevention for the specific target group(s) from WP2 and Selection of Regions, municipalities and local communities and identification of key stakeholders.
Stage 2: Group Model Building and Systems Mapping
Recruitment of key leaders and local stakeholders: A coordinator from participating SDC/regions and municipalities will together with the research team identify and recruit 12-15 key leaders (e.g. local politicians, department heads, municipality leaders) and local stakeholders (e.g. health care providers, local sport club representatives, religious leaders, NGOs within health and social care etc.). Key leaders and local stakeholders will be selected based on authority and capacity to initiate actions that are likely to prevent diabetes across sectors and organisations.
Group Model Building and systems mapping: During this stage, three workshops (WS1, WS2, WS3) will be held in each participating community. WS1 and WS2 will engage the key leaders and stakeholders. Local health profiles (based on data from the target groups found in WP2) will be presented to provide the first critical engagement step. The key leaders and stakeholders will map the system by building a causal loop diagram to understand how the perceived local system affects the diabetes development in their community. In WS3, all community members willing to engage in driving the change in the local system will be invited to identify priority areas for actions based on the causal loop diagram from WS1 and WS2.
Stage 3: Implementation of actions, support and monitoring
Actions and support: the output of WS3 is the formation of working groups across the sectors that will focus on implementing chosen actions. The working groups will be supported and supervised by a backbone office consisting of the regional and municipal coordinator(s) and the research team. A follow-up workshop (WS4) will be held with the key stakeholders six months after completion of WS3 to review the consolidated priority actions. To increase and maintain motivation and actions across region, municipality and community, subsequent follow-up meetings will be held with the working groups when needed during the follow-up period after WS3. Monitoring: At an annual meeting across region, municipality and community, health data will be presented to action groups, key leaders and stakeholders, to sustain and promote engagement. Evaluation
We will assess if the intervention and study procedures (WP4) are feasible by combining qualitative and quantitative data, focusing on practicality, acceptability, fidelity, and limited-effectiveness testing. Combined, these elements will give an essential understanding of what is required to upscale DP-Next to large-scale testing. The evaluation will be guided by recent frameworks(5,6) and will be constructed to allow for systematic documentation of processes and tentative outcomes. A final program theory on “what works for whom under what circumstances” based on the participatory systems dynamic approach will be made, including recommendations for large-scale testing. In addition to systems measurements, individual measurements will be collected in order to evaluate the specific actions (specific intervention components), e.g. changes in HbA1c, physical activity, diet patterns, sleep, general well-being, health literacy and social support.
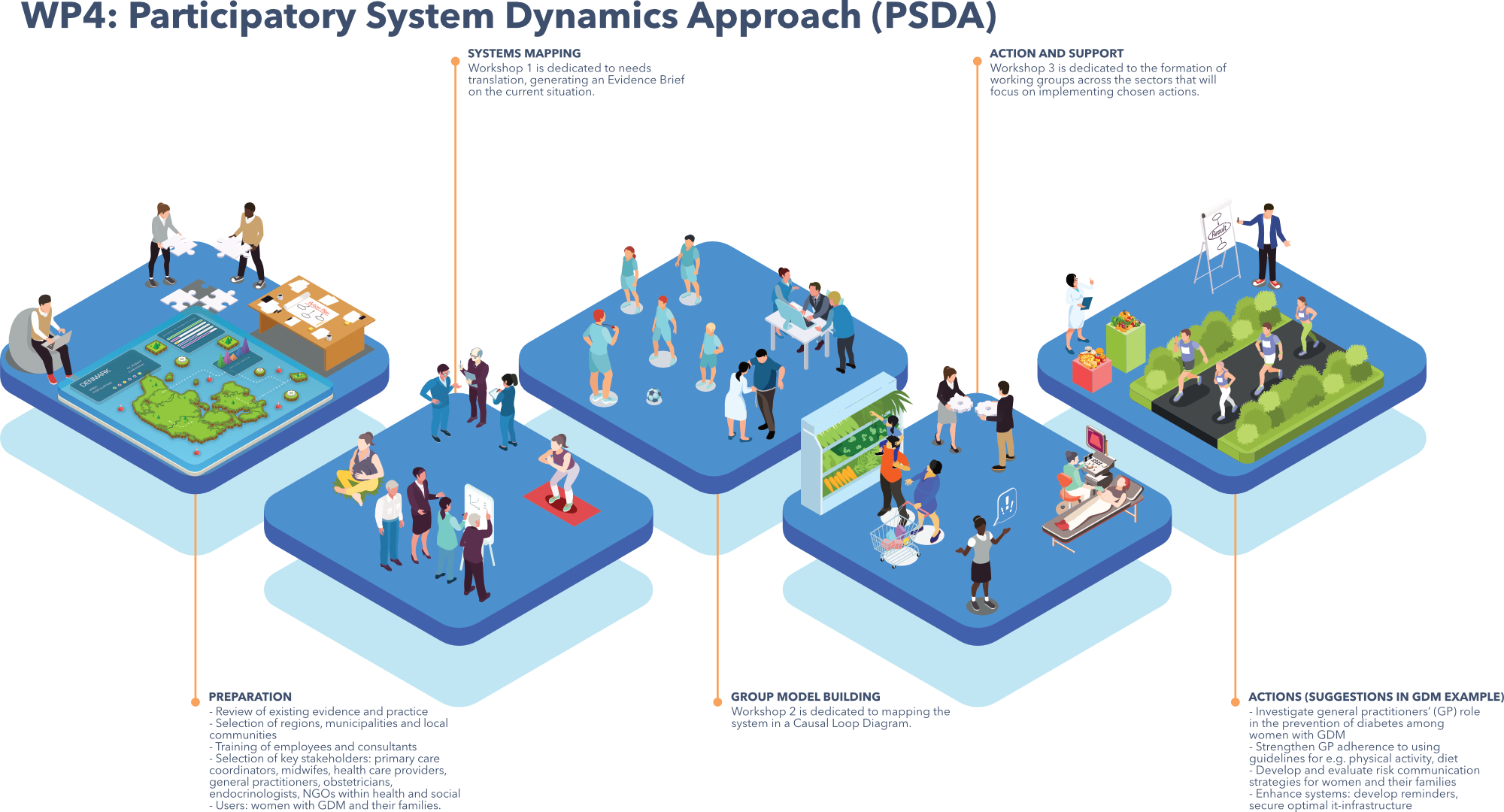
Example of PSDA in a high-risk target group.
To concretize the PSDA, the process is described in detail for a known high-risk group: ‘Women with a history of gestational diabetes (GDM)’. The same approach will be followed for other identified high-risk groups, ensuring that each group’s unique risks and needs are thoroughly assessed and addressed with the same rigour and systematic methodology.
Stage 1:
More than 3,500 (6%) pregnant women are annually diagnosed with GDM in Denmark and the number has increased 3-fold in the last decades(7). Women with GDM have an increased risk of long-term adverse health outcomes, including impaired glucose tolerance, T2D, and cardiovascular disease. GDM leaves the mother with an 8-10-fold higher risk of T2D, highest within 3-6 years after the GDM pregnancy(8,9). A recent Danish study found that almost 21% of women offered a clinical follow-up program, aiming at supporting women with GDM, had developed pre-diabetes, T2D or T1D one year postpartum(10). Studies have shown that T2D can be prevented or at least postponed by weight loss, physical activity, and diet(11–13). A low intensity family based intervention delivered in the first year after delivery in a Danish setting targeting women with prior GDM and their families showed improvements in a number of cardiometabolic risk factors, and was found acceptable and feasible for families and HCP (unpublished data for the FACE-IT study(14)). Although regular participation in follow-up screening at GP (recommended guidelines) has been shown to increase the likelihood of early detection of prediabetes/T2D, participation is low(10). Qualitative research has shown the use of electronic reminders of follow-up screening after GDM to be well received by women, although the interaction with their GP played a significant role(15) and that there is remaining need for support from healthcare providers for healthy lifestyle modifications adapted to their situation(16). Thus, the follow-up of women with GDM in general practice is not systematic, and hence, prevention of diabetes is suboptimal.
Stage 2:
The PSDA-example builds on this improvement potential by optimising the clinical follow-up in general practice using PSDA. Potential participants in the GMB process and system mapping (WS1-3) could potentially be: GP´s, families where the mother has been diagnosed with GDM, midwives, health visitors, obstetricians, endocrinologists, NGO´s and primary care coordinators.
Stage 3:
Based on the system mapping, working groups will be created and actions will start to be developed aiming to increase participation in the clinical follow-up visits at the GP. Thus it could be suggested that women with previous GDM could have a fasting blood glucose and an HbA1c taken postpartum at the 3-months child examination at the GP in order to follow the current Danish guidelines. In addition the woman will be reminded to have an HbA1c taken yearly also in alignment with the current guidelines. Examples of possible actions/interventions could be: To develop and evaluate risk communication strategies for GP´s to women with prior GDM and their families in order to increase continued participation. To enhance systems supporting the data-infrastructure, e.g. by using reminders(15) and platforms to access data (e.g. existing systems like SAMBLIK and alike).